June 30, 2025
How to Start a Paramedical Institute in India
June 06, 2025
Top Paramedical Franchise Options in India: Courses, Institutes, Career & Business Ideas
April 16, 2025
इम्यूनोहिस्टोकैमिस्ट्री (IHC): हिस्टोलॉजीमेंएकअद्वितीयतकनीक
April 09, 2025
Eco-Friendly Housekeeping: Sustainable Practices for Hotels
March 28, 2025
Eco-Friendly Home Improvements to Save Energy
March 25, 2025
हर्निया: कारण, प्रकार और उपचार
March 10, 2025
New Fermented Beverage
February 27, 2025
ऊतककाफ्रोजनसेक्शन (Frozen Section of Tissue)
February 25, 2025
Latest Advancements in Automatic Equipment Used in Hotel Front Offices
February 07, 2025
मलेरिया परजीवी: एक गंभीर स्वास्थ्य समस्या
February 06, 2025
वायरस अपनी संरचना (मॉर्फोलॉजी) क्यों बदलते हैं?
February 04, 2025
Degree in Radio Imaging Technician Course- What All the Course Covers?
January 31, 2025
Degree in Operation Theatre Technician Course- Employment and Career Opportunities
January 27, 2025
Benefits of Degree in Medical Laboratory Technician Course
January 25, 2025
MRI Safety: Important Guidelines for Patients
January 22, 2025
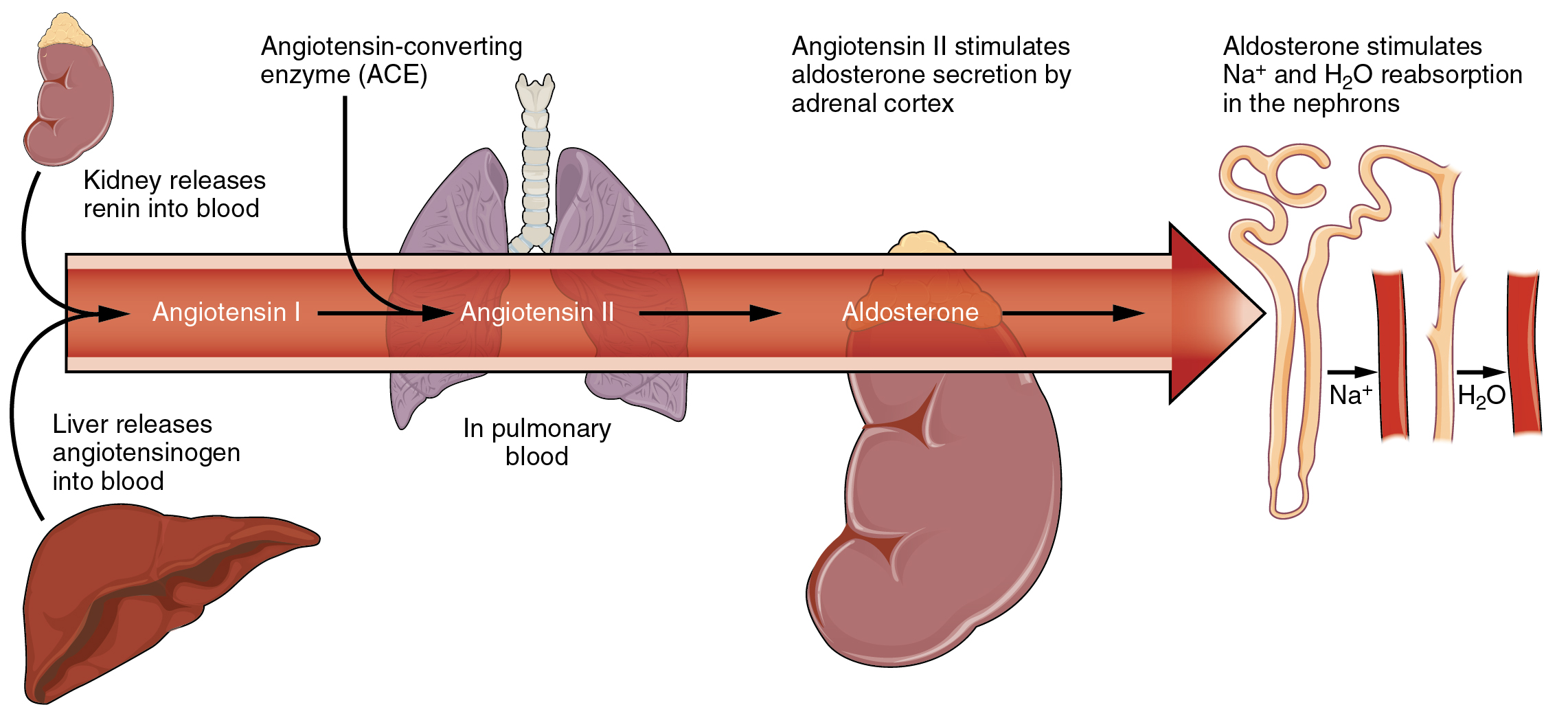
Renin-Angiotensin Regulation: Key to Blood Pressure and Fluid Balance
January 15, 2025
Diploma in Operation Theatre Technician Course- An Overview
January 07, 2025
New Trends in Non-Alcoholic Beverages: What is Shaping the Future?
January 06, 2025
Medical Lab Technician Course- What do MLTs do?
January 04, 2025
Schizophrenia
December 28, 2024
Hotel management course years duration- Gear-Up for A Career in Hotel Management Industry
December 21, 2024
Hospitality Management Course- An Ideal Career Option!
December 20, 2024
Cerebral palsy
December 16, 2024
Three Factors That Influence Hotel Management Course Fees
December 11, 2024
Dengue Symptoms and Clinical Diagnosis
December 01, 2024
Radioimmunoassay (RIA): A Revolutionary Biological Technique
November 30, 2024
Understanding the Mantoux Test: A Key Tool for Tuberculosis Diagnosis
November 24, 2024
Aplastic Anemia
November 21, 2024
The Presentability Playbook: A Guide to Excellence in Hospitality
November 15, 2024
The Double Marker Test
November 14, 2024
Laboratory Safety Precautions
November 08, 2024
Role of Operation Theatre Technician: Assisting in surgeries in hospitals
November 07, 2024
Origin and History of the Chandipura Virus
November 06, 2024
Infant Radiography
November 05, 2024
Epilepsy
October 26, 2024
Radiology Technician Course: Prepares you for a significant role in the healthcare industry
October 25, 2024
Operation Theatre Technician Course – Who are OT Technicians and What They Do?
October 24, 2024
Hotel Management Course – The Role of the Institute in Training Aspirants!
October 23, 2024
HLA (Human Leukocytes Antigen)
October 23, 2024
Hepatocellular Carcinoma
October 22, 2024
Stool Examination
October 18, 2024
Microscopic Examination of Cancer Cells
October 16, 2024
Personnel Monitoring Devices in Radiology
October 14, 2024
The Importance of Empathy in Paramedical Students
October 13, 2024
SUSTAINABLE PRACTICES IN HOTEL INDUSTRY
October 11, 2024
CREATININNE & KFT
October 07, 2024
The Importance of Professional Behaviour and Interdisciplinary Teamwork in Paramedical Students
September 25, 2024
Tap the Benefits of Studying B Voc in X-ray Technology
September 24, 2024
B.Voc in Hotel Management: A Degree Course for Aspiring HM Professionals
September 23, 2024
B Voc in Operation Theatre Technology: Learn About Objectives, Eligibility Criteria, and Salary